Cases include four defendants charged in this district involving over $129 million
September 18, 2021 - SAN DIEGO – A strategically coordinated, six-week nationwide federal law enforcement action has resulted in criminal charges against 138 defendants, including 42 doctors, nurses, and other licensed medical professionals, in 31 federal districts across the United States for their alleged participation in various health care fraud schemes that resulted in approximately $1.4 billion in alleged losses.
The enforcement action includes criminal charges against four defendants here in the Southern District of California, involving more than $129 million in intended losses.
Nationwide, this action includes more than $1.1 billion in fraud committed using telemedicine, more than $29 million in COVID-19 health care fraud, more than $133 million connected to substance abuse treatment facilities, or “sober homes,” and more than $160 million connected to other health care fraud and illegal opioid distribution schemes across the country
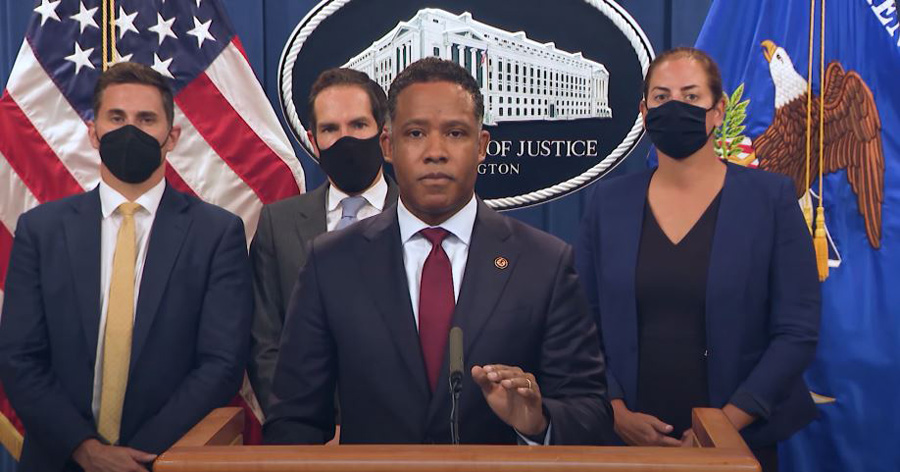
"Federal dollars devoted to care for the sick and suffering in our community should not be diverted to line the pockets of greedy opportunists,” said Acting U.S. Attorney Randy Grossman. “Now more than ever, we recognize the importance of our health care system and the important federal programs that care for elderly and Americans with disabilities."
“This nationwide enforcement action demonstrates that the Criminal Division is at the forefront of the fight against health care fraud and opioid abuse by prosecuting those who have exploited health care benefit programs and their patients for personal gain,” said Assistant Attorney General Kenneth A. Polite Jr. of the Justice Department’s Criminal Division. “The coordinated law enforcement actions announced today send a clear deterrent message and should leave no doubt about the department’s ongoing commitment to ensuring the safety of patients and the integrity of health care benefit programs, even amid a continued pandemic. I am proud of the hard work and dedication of those throughout law enforcement who are working to safeguard our health care system and our nation.”
Today’s enforcement actions were led and coordinated by the Health Care Fraud Unit of the Criminal Division’s Fraud Section, in conjunction with its Health Care Fraud and Appalachian Regional Prescription Opioid (ARPO) Strike Force program, and its core partners, the U.S. Attorneys’ Offices, the Department of Health and Human Services Office of Inspector General (HHS-OIG), FBI, and the Drug Enforcement Administration (DEA), as part of the department’s ongoing efforts to combat the devastating effects of health care fraud and the opioid epidemic. The Southern District of California worked with the Justice Department’s Criminal Division and agents from HHS-OIG, FBI, and DEA in the investigation and prosecution of these cases.
Telemedicine Fraud Cases
The largest amount of alleged fraud loss charged in connection with the cases announced today – over $1.1 billion in allegedly false and fraudulent claims submitted by more than 50 criminal defendants in 11 judicial districts nationwide – relates to schemes involving telemedicine: the use of telecommunications technology to provide health care services remotely.
The continued focus on prosecuting health care fraud schemes involving telemedicine reflects the success of the nationwide coordinating role played by the Fraud Section’s National Rapid Response Strike Force, the creation of which was announced at the 2020 National Health Care Fraud and Opioid Takedown. The National Rapid Response Strike Force helped coordinate the prosecution of the telemedicine initiative, Sober Homes initiative, and COVID-19 cases that were announced today. The focus on telemedicine fraud also builds on the telemedicine component of last year’s national takedown and the impact of the 2019 “Operation Brace Yourself” Telemedicine and Durable Medical Equipment Takedown, which resulted in an estimated cost avoidance of more than $1.5 billion in the amount paid by Medicare for orthotic braces in the 17 months following that takedown.
COVID-19 Fraud Cases
Nine defendants in the cases announced today are alleged to have engaged in various health care fraud schemes designed to exploit the COVID-19 pandemic, which resulted in the submission of over $29 million in false billings.
In the Southern District of California, Roselia Kubeck and Rosario Gonzalez pleaded guilty to having approached residents of senior complexes in El Centro and Calexico, California, who were Medicare beneficiaries, and offering COVID-19 screening tests for the residents. The defendants knew at the time that the tests would not actually test for COVID-19 but would be a general respiratory pathogens screening panel that tested for the presence of several kinds of respiratory pathogens. They also took urine samples from the Medicare beneficiaries without explaining that the urine samples were not necessary to conduct a COVID-19 test. The defendants then completed requisition forms for tests on the nasal swabs and urine samples, and inaccurately indicated on the forms that the beneficiaries needed the respiratory tests because they were suffering from acute respiratory infections and needed urine tests because the beneficiaries were long-term users of opiates or had urinary tract infections. The laboratories that performed the tests subsequently submitted inaccurate and medically unnecessary claims to Medicare based on the inaccurate diagnoses that the defendants put on the requisition forms.
The law enforcement action today also includes criminal charges against five defendants across the country related to the misuse of Provider Relief Fund monies. The Provider Relief Fund is part of the Coronavirus Aid, Relief, and Economic Security (CARES) Act, a federal law enacted March 2020 designed to provide needed medical care to Americans suffering from COVID-19.
The COVID-19 cases announced today build upon the success of the COVID-19 Health Care Fraud Takedown on May 26, a coordinated law enforcement action against 14 defendants in seven judicial districts for over $128 million in false billings. The law enforcement action and the cases announced today were brought in coordination with the Health Care Fraud Unit’s COVID-19 Interagency Working Group, which is chaired by the National Rapid Response Strike Force and organizes efforts to address illegal activity involving health care programs during the pandemic.
Sober Homes Cases
The sober homes cases are announced on the one-year anniversary of the first ever national sober homes initiative in 2020, which included charges against more than a dozen criminal defendants in connection with more than $845 million of allegedly false and fraudulent claims for tests and treatments for vulnerable patients seeking treatment for drug and/or alcohol addiction. The over $133 million in false and fraudulent claims that are additionally alleged in cases announced today reflect the continued effort by the National Rapid Response Strike Force and the Health Care Fraud Unit’s Los Angeles Strike Force, with the participation of the U.S. Attorney’s Offices for the Central District of California and the Southern District of Florida, to prosecute those who participated in illegal kickback and bribery schemes involving the referral of patients to substance abuse treatment facilities; those patients could be subjected to medically unnecessary drug testing – often billing thousands of dollars for a single test – and therapy sessions that frequently were not provided, and which resulted in millions of dollars of false and fraudulent claims being submitted to private insurers.
Cases Involving the Illegal Prescription and/or Distribution of Opioids and Cases Involving Traditional Health Care Fraud Schemes
The cases announced today involving the illegal prescription and/or distribution of opioids involve more than 13 defendants, including several charges against medical professionals and others who prescribed over seven million doses of opioids and other prescription narcotics. The cases that fall into more traditional categories of health care fraud include charges against 67 defendants who allegedly participated in schemes to submit more than $160 million in false and fraudulent claims to Medicare, Medicaid, TRICARE, and private insurance companies for treatments that were medically unnecessary and often never provided.
In the Southern District of California, Ronald Charles Green Jr. and Melinda Elizabeth Green were charged with conspiring to defraud TRICARE and Medicare out of more than $129 million. In connection with a compounding pharmacy fraud, the defendants allegedly engaged in a scheme involving the submission of false and fraudulent claims to TRICARE for expensive and medically unnecessary pain creams, scar creams and multi-vitamins, which were billed through compound pharmacies. Thereafter, the defendants allegedly launched multiple durable medical equipment companies, and carried out a scheme to defraud Medicare through the submission of false and fraudulent claims for expensive durable medical equipment which were induced through a system of illegal kickbacks. Out of the $129 million in claims, Medicare paid the defendants’ companies more than $69 million.
Prior to the charges announced as part of today’s nationwide enforcement action and since its inception in March 2007, the Health Care Fraud Strike Force, which maintains 15 strike forces operating in 24 districts, has charged more than 4,600 defendants who have collectively billed the Medicare program for approximately $23 billion. In addition to the criminal actions announced today, CMS, working in conjunction with HHS-OIG, announced more than 15 payment suspensions to decrease the presence of fraudulent providers.
The Southern District of California cases discussed herein were prosecuted by Assistant U.S. Attorneys Valerie Chu and Kevin Larsen and investigated by the Federal Bureau of Investigation, the Office of Inspector General for the United States Department of Health and Human Services, and the Defense Criminal Investigative Service. Grossman thanked the prosecutors and law enforcement agencies for working hard to achieve justice in these matters.
On May 17, 2021, the Attorney General established the COVID-19 Fraud Enforcement Task Force to marshal the resources of the Department of Justice in partnership with agencies across government to enhance efforts to combat and prevent pandemic-related fraud. The Task Force bolsters efforts to investigate and prosecute the most culpable domestic and international criminal actors and assists agencies tasked with administering relief programs to prevent fraud by, among other methods, augmenting and incorporating existing coordination mechanisms, identifying resources and techniques to uncover fraudulent actors and their schemes, and sharing and harnessing information and insights gained from prior enforcement efforts. For more information on the Department’s response to the pandemic, please visit https://www.justice.gov/coronavirus
Anyone with information about allegations of attempted fraud involving COVID-19 can report it by calling the Department of Justice’s National Center for Disaster Fraud (NCDF) Hotline at 866-720-5721 or via the NCDF Web Complaint Form at: https://www.justice.gov/disaster-fraud/ncdf-disaster-complaint-form.
*A complaint, information or indictment is merely an allegation, and all defendants are presumed innocent until proven guilty beyond a reasonable doubt in a court of law.
Source: DOJ Release









